Just as his energy was returning, Southern California was inundated with new, often fatal cases.
Garrett-Pate wished he could go to a blood bank to donate the enriched plasma coursing through his body.
“I potentially have something in me that could at least help someone recover,” he said. “Maybe prevent someone from dying. And yet simply because I am gay, I can’t do anything with it.”
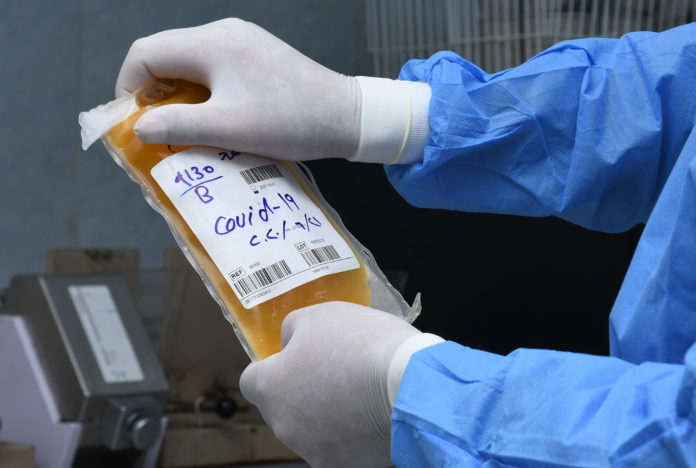
Liquid Gold
Garrett-Pate’s blood plasma, yellowish fluid filled with COVID-19 antibodies — tiny proteins designed to ward off future infections —is “liquid gold,” said Dr. Suchi Pandey, chief medical officer for Stanford Blood Center. “Plasma is essentially an important component of your blood to carry other stuff like antibodies through your body.”
Pandey says early results from clinical trials show that donated plasma from people who have battled COVID-19, a therapy known as convalescent plasma, is beneficial for other sick patients if it’s rich in antibodies and infused early in the course of the disease, when patients are experiencing mild symptoms.
The FDA has authorized the use of plasma for hospital patients only under these conditions, so the ideal time to donate is soon after someone recovers from COVID-19, because that’s when their antibody levels are highest.
That’s not always possible for gay men who are sexually active. They have to wait three months after a sexual encounter before donating blood or plasma.
“But someone who’s just as sexually active but not a man having sex with men can walk into any blood bank in America and give blood,” said Garrett-Pate.
A Lifetime. A Year. Then Three Months
During the AIDS crisis in the 1980s, the FDA determined it was too dangerous for sexually active gay and bisexual men to donate blood or plasma. That lifetime ban was lifted in 2015, provided the donor had been celibate a year.
But the pandemic has forced the cancellation of hundreds of thousands of blood drives, often hosted by schools or businesses, and by last spring, supplies had dwindled to critically low levels. So the FDA shortened the moratorium on giving blood to three months from the time a gay or bisexual donor last had sex.
Even though all donated blood is screened for HIV and other viruses, the agency says a celibacy window is still necessary. An FDA spokesperson wrote in an email that while blood supply screening “is highly sensitive, a small risk of HIV transmission still exists.”

Stigma or Science?
Critics say the policy isn’t based on evidence, but on homophobia.
“The FDA’s blood donation ban is 100% driven by fear, ignorance and outdated stereotypes about gay and bisexual men,” said California State Sen. Scott Wiener, D-San Francisco. “The federal government has an atrocious history over the last 40 years with HIV.”
Back in the 1980s, it took several months to know if someone had contracted HIV after a sexual encounter, but testing technology has dramatically improved over the years.
“We can very accurately detect the presence of HIV in patients about 10 days after HIV transmission occurs,” said Dr. Monica Hahn, an HIV specialist at UCSF.
She said requiring any amount of time without sex longer than 10 days isn’t necessary, so “there is absolutely nothing scientifically that justifies this ban.”
Questionnaire as Alternative
The FDA is considering swapping out the three-month celibacy requirement in favor of a risk questionnaire about a potential donor’s sexual activity. Anybody who is not monogamous — gay or straight — would have to wait before giving blood. Three of the nation’s largest blood centers, Vitalant, OneBlood and the American Red Cross, are launching a pilot study funded by the FDA to investigate the safety of switching to these questionnaires.
Garrett-Pate would gladly fill one out.
“All any of us want to do in life is help other people. Whether it’s donating blood, donating plasma,” he said. “We’re holding them back from making an impact on the world.”
The American Red Cross estimates that every two seconds, someone in the U.S. requires blood: accident or burn victims, heart surgery patients, organ transplant recipients … or people fighting COVID-19.