After more than two years of turmoil and stress during the COVID pandemic, here’s a bit of good news for the state’s public health system: Cases of monkeypox have plummeted in recent weeks.
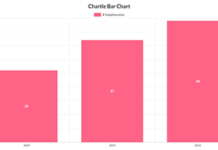
The state is now seeing just a handful of reported new infections per week, state epidemiologist Dr. Rachel Herlihy said. At the peak in mid-August, the state was recording more than 40 new cases per week. There have been a little more than 300 confirmed cases of monkeypox in Colorado this year, no deaths, nine hospitalizations and no cases of infection in children.
Herlihy called the trend, “a really nice steady decline.”
“That trend we’re seeing in Colorado is really mirroring what we’re seeing nationally,” she said.
The cause of the decline is not a mystery, Herlihy and another local expert say. Instead, it is a win for the state’s public health system, as well as a testament to the resolve of the state’s LGBTQ community to proactively take steps to minimize the risk of spread.
The most recent outbreak of monkeypox around the globe has been concentrated in the LGBTQ community, and Colorado is no exception. According to data from the Colorado Department of Public Health and Environment, 94% of Colorado’s cases have been among cisgender men, and 77% of cases have been among people who identify as gay or lesbian.
But there was no good reason why the outbreak wouldn’t spread more widely. The monkeypox virus — sometimes now referred to as MPV or MPXV, to avoid the stigma that comes with an association to monkeys — can be transmitted in a variety of ways, including some that do not require direct contact with an infected person. The primary transmission route in the current outbreak appears, so far, to have been through close contact during sex.
If the virus were to have jumped into a different social network — say, a prison or a child care center — there could have been a new surge in infections, said Dr. Daniel Pastula, an associate professor of neurology, infectious diseases and epidemiology at the University of Colorado and the Colorado School of Public Health. That made it vitally important to stop the virus early.
Pastula said it’s a credit to the state’s public health system that it set up a vaccination campaign so quickly and a credit to the LGBTQ community that it came together to educate its members on the virus.
“The LGBTQ community, particularly men who have sex with men, really stepped up to protect their health and work with public health authorities to get the word out about monkeypox,” Pastula said. “I think this would have been way worse without any intervention.”
A vaccine success story
Both Herlihy and Pastula said vaccination efforts likely had a huge impact in slowing the spread of monkeypox.
The state has administered roughly 18,000 doses of the vaccine to more than 12,000 people identified as being currently at highest risk of exposure. While initially limited, vaccine supplies have now improved, so much so that the state — along with health systems across the country — is able to use it proactively instead of reactively.
Early doses were only available for people with known or likely monkeypox exposures. (The vaccine, which is named Jynneos, can prevent someone from developing monkeypox if given after exposure.) But as supplies have improved, CDPHE has expanded the eligibility criteria several times with an aim of vaccinating more people before they are exposed to the virus.
Vaccination is now available to anyone who has had multiple or anonymous sexual partners, has had close physical contact with someone in a venue where anonymous or group sex may occur, has been diagnosed with gonorrhea or syphilis in the past six months, is living with HIV or who is eligible for HIV preventative medication known as PrEP. People who engage in commercial or transactional sex are also eligible, along with people who have had high-risk contact with someone who has monkeypox.
Data released last week by the Centers for Disease Control and Prevention found that men who were not vaccinated against monkeypox were 14 times more likely to contract the disease than those who were.
“Even after one dose, this looks like it’s a pretty good vaccine,” Pastula said.
Herlihy said most of the doses the state is administering now are second doses, aimed at providing longer-lasting protection, though first doses are still available.
A community response
Also important in reducing infections has been the actions of people in the LGBTQ community, Pastula said.
Another CDC study found that nationwide an estimated half of men who have sex with men reported reducing their number of sexual partners, new sexual partners and use of dating apps in response to the monkeypox outbreak.
Those changes followed sustained work by LGBTQ community organizations, working with public health agencies, to inform community members about the virus. Pastula said it represents a model for how to conduct a public health campaign — engaging with the community most affected without creating stigma or judgment.
“Getting the community that’s highest risk and getting them involved very much is limiting the spread of this,” he said. “I’m hopeful that the outbreak is now waning and it does not hop into new communities or social networks.”
The end of monkeypox … for now?
Herlihy also expressed optimism that the virus may be on its way out the door in Colorado. But she also warned against overconfidence.
“It’s tough to know where things are going to go from here,” she said. “It’s tough to know if we’re going to continue to see low levels of transmission.”
Monkeypox is a zoonotic disease, meaning it can be passed between animals and people through close contact. And it is endemic in parts of Africa, where it circulates among small mammals until another opportunity to infect people comes along. (A previous outbreak of monkeypox in North America involved pet prairie dogs.)
That means it’s unlikely monkeypox can be eradicated globally. But Pastual said there’s no evidence so far that the virus has found an animal reservoir in North America. That doesn’t mean it can’t continue spreading at low levels among people in Colorado before surging anew, though.
For that reason, Pastula said he recommends people at risk for exposure keep up their prevention strategies and continue getting vaccinated, if they haven’t already.
“It shows the importance of investing in our public health systems so we can detect outbreaks and respond to them quickly,” he said.