Monkeypox vaccine shortages threaten attempts to tackle the UK’s worsening outbreak, charities have warned, as cases “overwhelm” sexual health services.
In a statement on Tuesday, a coalition of sexual and public health organisations criticised the Government’s response and warned the virus risks becoming endemic unless the immunisation drive is “super charged”.
“The current vaccination rollout is too slow with far too few being vaccinated,” said the statement, from nine organisations including the British Association of Sexual Health & HIV, Association of Directors of Public Health and Terrence Higgins Trust.
“This is compounded by a lack of coordination between those who are responsible for its delivery and insufficient quantities of vaccine,” it added, warning that communication with affected communities “has been poor” and there are “no plans” to combat sub-optimal access.
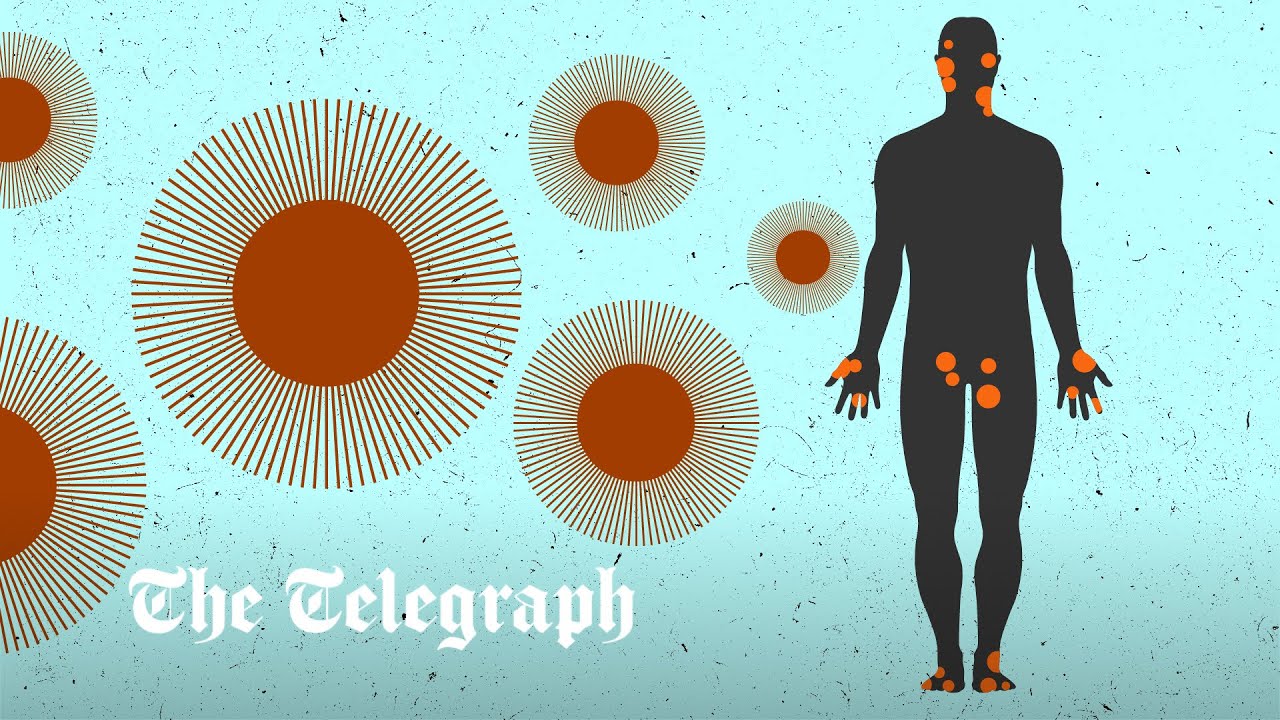
Across the globe, more than 9,780 confirmed and suspected cases have been reported since May in an unprecedented outbreak outside endemic regions. The UK has detected 1,735 cases, the vast majority in England among men who have sex with men.
According to the UK Health Security Agency, the outbreak is doubling every 15 days and undetected transmission is widespread – in almost 80 per cent of cases, there is no information about whether an individual has been in contact with a confirmed patient.
The UKHSA said it has “mobilised a large-scale national response”, and has procured almost 30,000 doses of the smallpox vaccine – which also protects against monkeypox.
“Sufficient vaccine supplies are available, enabling the NHS to roll out the programme to high risk groups,” said Dr Andrew Lee, a UKSHA incident director.
But the latest statement criticised a lack of transparency over Britain’s procurement plans and rollout, and claimed that the country will need to protect 125,000 people as the outbreak shows few signs of abating.
Richard Angell, campaigns director at Terrence Higgins Trust, said: “There is a clear choice in front of us: urgently do what is needed to tackle the spread of monkeypox or continue the lacklustre response to date which will mean the virus becomes endemic in the UK with more and more people impacted.”
The statement added that sexual health services are facing “unsustainable” pressures, which could disrupt efforts to tackle other diseases, including HIV. Although the virus is not a sexually transmitted infection, it can present like one, and the group called for £51m to strengthen the response.
Prof Paul Hunter, a professor of medicine at the University of East Anglia, said he would have viewed the concerns as “a bit over the top” in May or early June.
“But it is clear that even in the UK we are not getting on top of this epidemic and unlikely to with the current strategy… we need to get better at getting vaccine to contacts and make it easy for anyone who believes they are a contact to get vaccinated,” he told the Telegraph.
Dr Hugh Adler, an infectious disease expert at the Liverpool School of Tropical Medicine, added: “We have always had the tools – contact tracing and vaccination – to interrupt monkeypox transmission, and at the start of this outbreak I was quite relaxed and assumed that the public health response would have it sorted in no time.
“But the system, as it stands, has been unable to contact trace in a sufficiently timely manner.”
But others pointed blame at LGBT+ groups, accusing them of failing to issue advice to those at risk and “taking a huge bet on gay men’s health”.
“[The criticism is] completely unfair,” said Malcolm Clark, head of research at the LGB Alliance. The LGBT lobby groups… were utterly complacent and did next to nothing to stop the spread of this new and evolving virus.
“They spent almost all their time and energy complaining about stigmatising of gay men and denying the blatantly obvious that this virus was spreading disproportionately among gay and bisexual men.”
Meanwhile, the World Health Organisation said on Tuesday that it would reconvene a panel to determine whether the outbreak constituted a global health emergency next week, after declining to trigger its highest alert at the end of June.
Protect yourself and your family by learning more about Global Health Security