Horton, R. Offline: COVID-19 is not a pandemic. Lancet 396, 874 (2020).
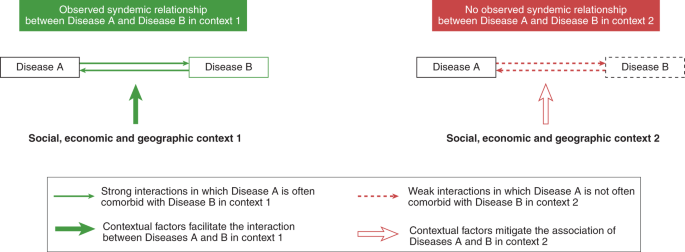
Mendenhall, E. The COVID-19 syndemic is not global: context matters. Lancet 30, 17848 (2020).
Islam, N. et al. Social inequality and the syndemic of chronic disease and COVID-19: county-level analysis in the USA. J. Epidemiol. Community Health 75, 496–500 (2021).
Singer, M., Bulled, N., Ostrach, B. & Mendenhall, E. Syndemics and the biosocial conception of health. Lancet 389, 941–950 (2017).
Gravlee, C. C. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am. J. Hum. Biol. 32, e23482 (2020).
Singer, M. C. Aids and the health crisis of the U.S. urban poor: the perspective of critical medical anthropology. Soc. Sci. Med. 39, 931–948 (1994).
Singer, M. Dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. Creative Sociol. 24, 99–110 (1996).
Stall, R. et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am. J. Public Health 93, 939–942 (2003).
Tsai, A. C. & Burns, B. F. O. Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept. Soc. Sci. Med. 139, 26–35 (2015).
Mendenhall, E. & Singer, M. What constitutes a syndemic? Methods, contexts, and framing from 2019. Curr. Opin. HIV AIDS 15, 213–217 (2020).
Rudd, K., Mair, C. & Angus, D. Applying syndemic theory to acute illness. JAMA 327, 33–34 (2022).
Gandhi, M., Spinelli, M. & Mayer, K. Addressing the sexually transmitted infection and HIV syndemic. JAMA 321, 1356–1358 (2019).
Tsai, A. C. Syndemics: a theory in search of data or data in search of a theory?. Soc. Sci. Med. 206, 117–122 (2018).
Link, B. G. & Phelan, J. C. Conceptualizing stigma. Annu. Rev. Sociol. 27, 363–385 (2001).
Ranney, M. L., Betz, M. E. & Dark, C. #ThisIsOurLane: firearm safety as health care’s highway. N. Engl. J. Med. 380, 405–407 (2019).
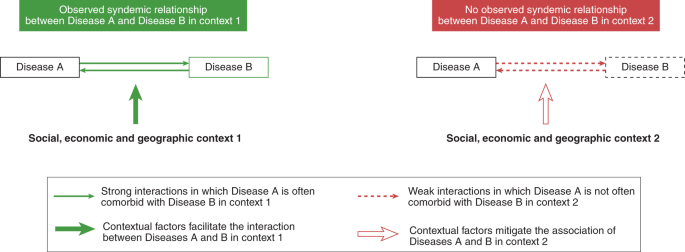
Tsai, A. C., Mendenhall, E., Trostle, J. & Kawachi, I. Co-occurring epidemics, syndemics, and population health. Lancet 389, 978–982 (2017).
Stall, R., Coulter, W. S., Reuel Friedman, R. & Plankey, W. M. Commentary on ‘Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept’ by A. Tsai and B. Burns. Soc. Sci. Med. 145, 129–131 (2015).
Tsai, A. & Venkataramani, A. Syndemics and health disparities: a methodological note. AIDS Behav. 20, 423–430 (2016).
Taft, T. & Keefer, L. A systematic review of disease-related stigmatization in patients living with inflammatory bowel disease. Clin. Exp. Gastroenterol. 9, 49–58 (2016).
Ghinai, I., Willott, C., Dadari, I. & Larson, H. J. Listening to the rumours: what the northern Nigeria polio vaccine boycott can tell us ten years on. Glob. Public Health 8, 1138–1150 (2013).
Wonodi, C. et al. Conspiracy theories and misinformation about COVID-19 in Nigeria: implications for vaccine demand generation communications. Vaccine 40, 2114–2121 (2022).
Dhanani, L. Y. & Franz, B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health 207, 31–38 (2022).
Corona, G. et al. Diabetes is most important cause for mortality in COVID-19 hospitalized patients: systematic review and meta-analysis. Rev. Endocr. Metab. Disord. 22, 275–296 (2021).
Jindal, H. A. et al. Higher coronavirus disease-19 mortality linked to comorbidities: a comparison between low-middle income and high-income countries. J. Educ. Health Promot. 10, 377 (2021).
Remien, R. H. et al. Mental health and HIV/AIDS: the need for an integrated response. AIDS 33, 1411–1420 (2019).
Mendenhall, E., Kohrt, B. A., Norris, S. A., Ndetei, D. & Prabhakaran, D. Non-communicable disease syndemics: poverty, depression, and diabetes among low-income populations. Lancet 389, 951–963 (2017).
Ikeda, D. J., Kidia, K., Agins, B. D., Haberer, J. E. & Tsai, A. C. Roll-out of HIV pre-exposure prophylaxis: a gateway to mental health promotion. BMJ Glob. Health 6(12), e007212 (2021).
Logie, C. H. et al. A longitudinal study of associations between HIV‐related stigma, recent violence and depression among women living with HIV in a Canadian cohort study. J. Int. AIDS Soc. 22(7), e25341 (2019).
Metzi, J. M. & Hansen, H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc. Sci. Med. 103, 126–133 (2014).
Mendenhall, E. Syndemic Suffering: Social Distress, Depression, and Diabetes among Mexican Immigrant Women (Routledge, 2012).
Mendenhall, E. Beyond comorbidity: a critical perspective of syndemic depression and diabetes in cross-cultural contexts. Med. Anthropol. Q. 30, 462–478 (2015).
Logie, C. H., James, L., Tharao, W. & Loutfy, M. R. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 8(11), e1001124 (2011).
McDaid, L. M. et al. Informing theoretical development of salutogenic, asset-based health improvement to reduce syndemics among gay, bisexual and other men who have sex with men: empirical evidence from secondary analysis of multi-national, online cross-sectional surveys. SSM Popul. Health 10, 100519 (2019).
Schwartz, S. R. et al. The immediate effect of the Same-Sex Marriage Prohibition Act on stigma, discrimination, and engagement on HIV prevention and treatment services in men who have sex with men in Nigeria: analysis of prospective data from the TRUST cohort. Lancet HIV 2, E299–E306 (2015).
Ogunbajo, A. et al. Poor sleep health is associated with increased mental health problems, substance use, and HIV sexual risk behavior in a large, multistate sample of gay, bisexual and other men who have sex with men (GBMSM) in Nigeria, Africa. Sleep Health 6, 662–670 (2020).
Ogunbajo, A. et al. Experiences of minority stress among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa: the intersection of mental health, substance use, and HIV sexual risk behavior. Glob. Public Health 16, 1696–1710 (2021).
Poteat, T. C., Logie, C. H. & van der Merwe, L. L. A. Advancing LGBTQI health research. Lancet 397, 2031–2033 (2021).
Scheim, A. I., Perez-Brumer, A. G. & Bauer, G. R. Gender-concordant identity documents and mental health among transgender adults in the USA: a cross-sectional study. Lancet Public Health 5, 196–203 (2020).
Hatzenbuehler, M. L. et al. Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: a quasi-natural experiment. Am. J. Public Health 102, 285–291 (2012).
Huang, Y.-T. & Liang, Z. Effects of same-sex marriage legalization for sexual minority men in Taiwan: findings from a prospective study. Int. J. Public Health 67, 1604489 (2022).
Judiciary Committee, Education and Employment Committee, Harding & Grall. CS/CS/HB 1557: Parental Rights in Education (The Florida Senate, 2022).
Karmacharya, R., Kieling, C. & Mondelli, V. Integrating stem cell-based experiments in clinical research. Eur. Psychiatry 63, e62 (2020).
Mendenhall, E. et al. A mixed-methods, population-based study of a syndemic in Soweto, South Africa. Nat. Hum. Behav. 6, 64–73 (2022).
Organista, K., Jung, W. & Neilands, T. A structural–environmental model of alcohol and substance-related sexual HIV risk in Latino migrant day laborers. AIDS Behav. 24, 3176–3191 (2020).
Safren, S. A. et al. Addressing syndemics and self-care in individuals with uncontrolled HIV: an open trial of a transdiagnostic treatment. AIDS Behav. 24, 3264–3278 (2020).
Bhardwaj, A. & Kohrt, B. A. Syndemics of HIV with mental illness and other noncommunicable diseases: a research agenda to address the gap between syndemic theory and current research practice. Curr. Opin. HIV AIDS 15, 226–231 (2020).