As a nation, we must not ignore diseases as they spread around the world, because we know that viruses don’t respect political borders. We must demand that our elected leaders continue to make responding to these viruses a priority. It was alarming when Congress lost interest in funding our nation’s Covid response while the pandemic continued. And now, at a time when our underfunded public health workforce is exhausted, we must rally to confront yet another virus with monkeypox spreading throughout the nation.
In responding to monkeypox we must be honest and transparent but cognizant of the risks and realities faced by LGBTQ Americans. We have already seen a resurgence of fear and hatred toward the LGBTQ community — fueling a stigma that can tie public health messaging in knots. Some worry that highlighting at-risk communities could lull others into a place of complacency, and that the simple association with the gay community could stoke acts of violence. The CDC lacks any reference to gender or sexual orientation on its webpage addressing monkeypox vaccination, but the data is clear: Gay, bisexual and other men who have sex with men (MSM) are currently at highest risk for becoming infected.
In North Carolina, our motto is “to be rather than to seem.” To me, that means get to work and continuously improve as you go.
Before our first reported case on June 23, we were ready. We were prepared to test for monkeypox at our state lab, we gave guidance to healthcare providers and we planned for vaccine distribution. By July 6, limited doses of the vaccine began arriving and we had already set up regional vaccine locations around the state with local health departments. On July 14, we published a detailed response plan describing for providers, community organizations and the public our approach to testing, treatment, vaccination and sharing information.
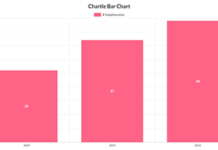
From the start, we were clear that data would drive our response and our message. We’ve published daily case numbers on our website, and as soon as we had sufficient numbers to protect privacy, we published demographic information about cases and vaccines. On Aug. 10, we released one of the first equity analyses in the nation, finding that while 70 percent of monkeypox cases in North Carolina were in Black men, less than a quarter of vaccines had gone to Black individuals. Our report offered key actions we and our partners in North Carolina are taking to improve, like working with party promoters to have vaccination events onsite.
As North Carolina’s state health secretary, I care deeply about protecting people’s health. And to me, this is also personal.
Here are the five things we need most right now in our national response:
First, data must drive the response. Anyone can get monkeypox, but right now nearly all cases are in men who report recent sexual contact with men. That’s why we must prioritize the MSM community, especially with the limited vaccine supply, while using empathetic messages to help destigmatize the disease.
As we organize our operational response, it is non-negotiable for state health departments to collect and share detailed demographic data with the public, so that we can understand the impact on different communities and close equity gaps.
Second, state and local health departments must partner with LGBTQ organizations to organize outreach to MSM, share information, answer questions and provide vaccines — fast. The city of Charlotte, the epicenter of North Carolina’s outbreak, celebrated Pride last weekend. I’m proud that we muscled together a partnership to deliver vaccines at the event, with support from all levels of government along with local organizations. This strategy can be replicated at other events and locations that serve the LGBTQ community.
Third, more is needed from health care providers. Medical professionals should test anyone with unexplained sores or lesions, including those from outside the MSM community, so we can stay ahead of the spread of this virus. Providers should educate themselves about appropriate infection control protocols and navigate them with empathy and care for the patient, just as they would with other infectious diseases, such as strep throat. When a patient has monkeypox, be persistent to work through the current federal process to get treatment. And finally, to help get folks vaccinated faster, providers and clinics serving the MSM community can go through their medical records and proactively reach out to their patients eligible for the vaccine and offer them advice.
Access to vaccines needs to be fast, easy and confidential. Appointment scheduling must be online, not just by phone. Clinics must co-locate with other routine health services, so no one knows why someone is in line. Instead of asking a long list of invasive vaccine eligibility questions, just ask: “Considering all the criteria, do you qualify?”
Fourth, while I’m encouraged that the federal government has declared monkeypox a public health emergency and assembled an experienced team to lead a national response, there are additional steps that the federal government needs to take. Start with cash. Making existing CDC Covid funding and FEMA disaster dollars available for monkeypox will allow states and localities to use the contact tracing and vaccine infrastructure that was built for Covid. HHS can issue a PREP Act emergency declaration to get pharmacists ready to vaccinate. We must also develop new test collection methods to move past painfully swabbing lesions and make those tests easier to use in mobile spaces and less reliant on health care staff. And of course, we need to continue to increase the supply of vaccines.
TPOXX, an antiviral treatment for smallpox that is being used to treat monkeypox, can be very hard to get. I applaud the federal government for improving the process for obtaining it. They need to continue to tweak that process to make it easier for providers and patients to get it quickly. They must also work rapidly to build the data necessary to understand if TPOXX could be authorized for emergency use and deployed in normal channels. As long as the process remains cumbersome, many providers and patients will simply go without.
Many people I know are scared, confused and being treated as diseases instead of human beings. People need help. Our workforce and healthcare system are tired and stretched. Our elected leaders in Congress need to refocus on bolstering our public health infrastructure. But we learned a lot over the past three years, and we have the tools and experience to successfully respond to this virus.
For now, instead of playing the blame game, let’s get down to business.