:quality(100)/cloudfront-us-east-1.images.arcpublishing.com/thesummit/4HZ4ODRV4ZFIJJBWS2E2FZRZMU.jpg)
When the monkeypox outbreak began this year, the world had a head start — many governments had vaccines for the virus in hand, in sharp contrast to the early days of the coronavirus pandemic.
But that early advantage hasn’t been fully seized. In the U.S., the government has been slow to get vaccines into the arms of those at highest risk, prolonging the suffering of gay men and those in their sexual networks and missing opportunities to contain the virus’ rampant spread. And there still isn’t a supply of the vaccine in Africa, where the current outbreak began and where several countries are grappling with rising cases and deaths.
In short — just as with testing — the United States and many other developed nations have failed to act on the painful lessons learned during covid, missing crucial opportunities to limit another looming global health crisis, experts told Grid. The Biden administration’s decision Thursday to declare a monkeypox public health emergency could give the government greater flexibility in funding its fight against the virus, including increasing the nation’s stock of vaccines and drugs. But that won’t immediately solve the current problems.
“We needed to completely rethink governance of public health emergencies in the United States” after covid, said Ali Khan, former director of the Office of Public Health Preparedness and Response at the Centers for Disease Control and Prevention. “It should’ve been a wake-up call.” Instead, he said, “We’re hitting the snooze alarm one more time. I find it inexplicable that efforts were not made immediately to redeploy these vaccines.”
ADVERTISEMENT
Currently, the federal government has shipped about 602,000 doses of vaccine — far short of what’s needed to vaccinate the estimated 1.6 million people the CDC deems as highest risk.
The urgency that comes with an emergency declaration will help energize the public health response and possibly contain the virus in the U.S., which has now infected more than 6,600 people. But by failing to quickly use existing tools, officials missed an opportunity to address the outbreak head-on in Africa and then as it spread around the world.
“I am glad they declared a public health emergency to ensure maximum flexibility to expedite the rollout of vaccines,” said Jennifer Nuzzo, an epidemiologist at Brown University. “I do think that greater urgency earlier could have greatly mitigated the spread of this virus.”
Before the current outbreak began, millions of vaccine doses sat in warehouses and stockpiles across North America and Europe, a fail-safe in case of a smallpox bioterror attack or pandemic. In 2017, when Nigerian scientists noticed worrying signs that monkeypox was spreading more rapidly among humans, some of those doses could’ve been deployed. But they weren’t.
In early May, when cases were exploding across Europe, primarily among gay and bisexual men, the United States could’ve released hundreds of thousands of doses it was storing in a Danish warehouse. But again, doses weren’t mobilized.
ADVERTISEMENT
Best-laid plans
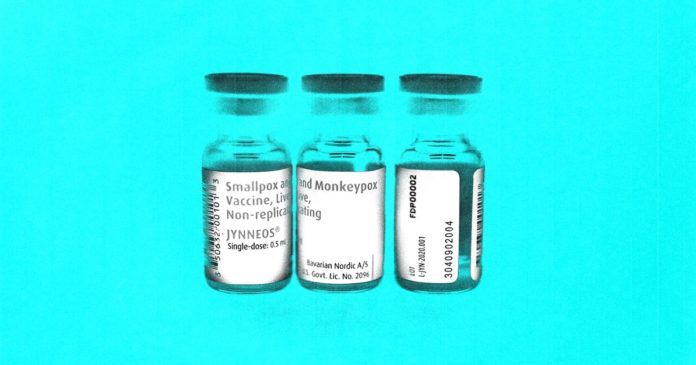
The globe has two main vaccines in its monkeypox arsenal. Both were designed to guard against smallpox, and both work against monkeypox, which is part of the same family of viruses. But the similarities stop there.
There’s significantly more of the older vaccine, ACAM2000. The United States has some 100 million doses in its national stockpile, ready for the worst-case scenario of a bioterror attack. Other countries likely have millions more doses. But ACAM2000 is a comparatively gnarly vaccine, housing an active vaccinia virus that’s delivered via numerous pokes of a two-pronged needle. (Most vaccines in common use today use an inactivated virus, or no virus at all, as with covid mRNA vaccines.) That live, though weakened, virus comes with side effects. About six in every 1,000 recipients experience heart inflammation, and the vaccine can be harmful to people with impaired immune systems, including those who have HIV — about a third of monkeypox cases. For smallpox, which can kill about 30 percent of people it infects, that trade-off makes sense, but it doesn’t for the much less lethal monkeypox virus.
A newer vaccine, Jynneos, is manufactured by a small Danish pharmaceutical company, Bavarian Nordic. The upside is that Jynneos is much milder than the older vaccine, and Food and Drug Administration-approved for monkeypox even in immunocompromised people. The downside is that there’s much less of it. Still, in 2014 the U.S. had about 20 million doses in the strategic national stockpile to help supplement ACAM2000 in case of a bioterror attack.
“The U.S. was uniquely well prepared to confront a monkeypox outbreak,” said Jay Varma, a physician and epidemiologist who specializes in infectious diseases at Weill Cornell Medical School. “We had already stockpiled both the original smallpox vaccine as well as a more modern, safer alternative,” he said.
But that preparation has not translated well into action, largely because federal officials were slow to respond to clear warning signs.
ADVERTISEMENT
The U.S. stockpile of 20 million dwindled to just 2,400 doses this year, the result of federal officials deciding to not replenish doses after they expired, which happens after about three years. Instead, the U.S. was investing in the development of a freeze-dried version of the vaccine that lasted longer. But FDA-approval delays and other factors slowed that process, according to a New York Times report.
In 2020, the U.S. ordered 1.4 million more liquid-frozen doses, which were stored in Denmark. But in late May, when monkeypox cases began popping up in the U.S., federal officials allowed about 215,000 of those ready-to-go doses to be delivered to European countries, according to a New York Times report.
“Even though there were explosive outbreaks occurring in major European cities in the early and mid May, the U.S. appears to have not made a sustained and intensive effort to release those vaccines here in the United States,” Varma said. “Any time you fall even a little bit behind in an infectious disease outbreak, it takes much more effort to catch up than if you had responded quickly from the beginning.”
Currently, the U.S. has delivered just over 602,000 doses of Jynneos, which it’s allocating to states based on estimated need. The U.S. only has enough vaccines in hand to cover about one-third of the 1.6 million gay and bisexual men the CDC deems at highest risk. The next batch of Jynneos from Bavarian Nordic won’t arrive until September, officials estimate.
On Thursday, FDA Commissioner Robert Califf announced the agency is considering enabling providers to deliver the vaccine intradermally, instead of under the skin, allowing each vial to supply up to five separate doses instead of one.
Fixing the supply chain is only a first step
But having more doses won’t solve the problem of getting those shots to people who need them. “Even after the U.S. resolves its vaccine supply problem, there is still going to be a major delivery problem,” Varma said. State and local public health departments are the backbone of vaccination efforts, but those departments are underfunded, understaffed and burnt out from the covid pandemic.
“Even the most well-resourced departments, like in New York City, are having trouble getting vaccines to people as quickly as they could,” he said. Problems with figuring out where to administer vaccines and which staff can administer them, as well as keeping track of vaccinations, have hampered the initial response.
“It’s a system that basically favored people with the technical savvy, as well as the time and ability to skip out on their jobs to get appointments first,” Varma said. “You can only imagine what it’ll be like when this epidemic spreads to more and more communities around the United States where their health departments don’t have anywhere near the same capacity.”
States’ responses to the outbreak have varied widely. “Georgia’s state health commissioner did not ever request all of the vaccines that were initially allocated to us,” said Melanie Thompson, an HIV physician and researcher in Atlanta and past chair of the HIV Medicine Association. “This has greatly hampered our response.” Additionally, the state has no dashboard on cases or vaccine recipients that would help guide an equitable distribution of vaccines, Thompson said. In Georgia, “the large majority of people with monkeypox are Black, and at least half have HIV,” she said. “Data should provide a road map to tell us where to offer services. Without data, we are blind to where the epidemic is and where it is going.”
By contrast, New York declared a state disaster emergency in response to the monkeypox outbreak there last week, which broadened the pool of people who can administer vaccines and requires providers to share data with state officials.
ADVERTISEMENT
If the U.S. deploys its limited vaccines in a targeted way to those most at risk — right now, queer men and their sexual networks, especially individuals with many sexual partners — the upward trend in cases can be turned around, said Alyssa Bilinski, an infectious disease modeler at Brown University. Nearly 500,000 men who have sex with men are at highest risk for monkeypox, Bilinski and her colleagues estimate, and if roughly 25 to 50 percent of them are vaccinated, the exponential spread of the outbreak could be quelled, according to a preprint released Tuesday. That percentage goes down if other control measures, like testing and contact tracing, become more robust.
“We are still in a position where a really good response is possible,” Bilinski said. “We should do everything we can to not miss that window by increasing supply and targeting communities who need the vaccine.”
That mobilization will take money and engagement with organizations focused on sexual health or serving LGBTQ communities. Many of these organizations are already working to address the crisis, but will need additional funding to meet the challenge. “None of this happens without money,” said Varma. “I’m somewhat pessimistic because we’ve seen the difficulty of mobilizing new funding in Congress at this time with covid.”
Beyond U.S. borders
There’s a chance the global spread of monkeypox could have been avoided, along with much suffering in Africa, had the international community responded to warning signs a few years ago.
Monkeypox is endemic in about a dozen African countries and has sparked small outbreaks since the 1970s, primarily tied to limited spillover from animals. But in 2017, Nigerian scientists started seeing more cases that were spreading differently, primarily among men. Nigerian public health officials requested help from other countries to investigate and address the outbreak but didn’t receive much. The situation in Nigeria “should have triggered some concern and effort to make sure that there was enough vaccine,” Khan said, both in Nigeria and other countries.
ADVERTISEMENT
But no vaccines came. Now, despite having the overwhelming majority of monkeypox deaths — 103 — and nearly 3,000 confirmed or suspected cases, the continent has yet to receive any doses.
“It is not surprising that we’re seeing the same thing happen with monkeypox that happened with covid-19,” said Olusoji Adeyi, a global health expert and president of Resilient Health Systems, a global health organization. “The fundamental factors that led to inequity in access to vaccines have not gone away. … This is one of the gross and deeply entrenched failures in global health.”
The structural factors that produce this inequity are large and varied, Adeyi said, including a concentration of vaccine manufacturers in North America and Europe, fiercely guarded intellectual property rights that shield pharmaceutical companies from sharing technology, and the hoarding of doses by wealthier countries. The vast stockpiles of ACAM2000 and Jynneos are largely located in the Global North.
The World Health Organization has said that it’s developing a vaccine-sharing mechanism for monkeypox, as it did with covid, but has released few specifics. Before the monkeypox outbreak, wealthy nations pledged 31 million doses of smallpox vaccine for use by the WHO in a time of international need, though it’s unclear what’s happening with those doses. “Experience teaches us not to put too much faith in pledges,” Adeyi said. “An approach that is based on charity and the goodwill of wealthy countries is not the way to achieve equity in global health.”
To succeed, the WHO’s program will have to improve on the structural problems that plagued Covax, the covid vaccine-sharing program that gave wealthy nations more leverage by allowing wealthy nations to simultaneously make unilateral purchases, Adeyi said. But whatever the nature of the program, it will have a lot of catching up to do.
ADVERTISEMENT
“Had there been greater global attention to this, when [monkeypox] was limited to a few countries in Western and Central Africa, perhaps the world as a whole would have been better prepared to deal with it more swiftly or robustly,” Adeyi said.
Thanks to Lillian Barkley for copy editing this article.