The global monkeypox outbreak is primarily being driven by sex between men, according to the first major peer-reviewed paper to analyze a large set of cases of the virus.
The outbreak, which epidemiologists believe initially began in mid-spring gatherings of gay and bisexual men in Europe, has since alarmed such experts by ballooning to nearly 16,000 cases worldwide.
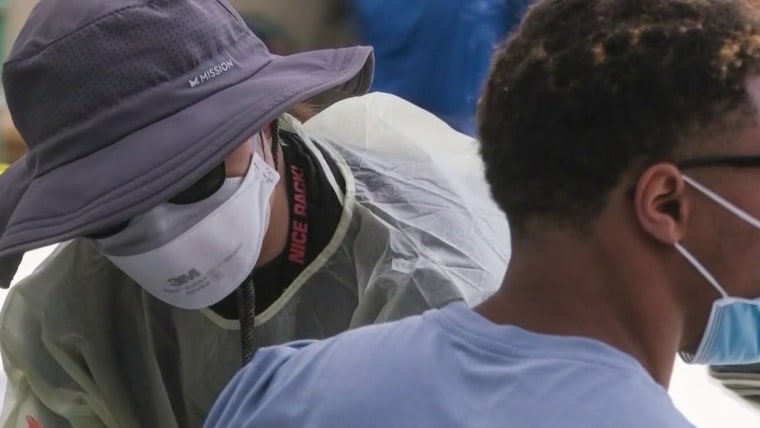
Now infectious disease specialists are developing an increasingly refined understanding of the predominant conduits of monkeypox transmission, as well as the typical disease course patterns.
“These data point clearly to the fact that infections are so far almost exclusively occurring among men who have sex with men,” said Jennifer Nuzzo, an epidemiologist at Brown University, of the new study, which was published Thursday in the New England Journal of Medicine. “And the clinical presentation of these infections suggest that sexual transmission, not just close physical contact, may be helping spread the virus among this population.”
“This large, multicountry study provides the most complete set of clinical and demographic data on monkeypox cases occurring outside endemic areas,” said Nuzzo, who was not involved with the study.
No one has died of monkeypox infection outside of Africa during this outbreak. And for many people, the disease is relatively mild and resolves on its own in a few weeks without any need for medical intervention. However, the new paper reports that monkeypox can cause pain so intense that a substantial proportion of people with the virus require hospitalization for pain management.
“We have seen patients with severe rectal pain that worsens every time they go to the bathroom, genital pain every time they urinate and throat pain every time they swallow,” said Dr. Jason Zucker, an infectious disease specialist at Columbia University Department of Medicine.
In the United States, confirmed cases of monkeypox have increased dramatically in recent weeks, to 2,593 as of Thursday. With fears mounting among infectious disease experts that the virus will become endemic in the U.S. and around the world, the Biden administration has been subject to intense criticism by activists and the public health community that its health agencies failed to act quickly enough to stem the outbreak.
The recent sharp rise in U.S. monkeypox diagnoses could be driven in part by increased testing, especially after the Centers for Disease Control and Prevention brought onboard five commercial testing companies during the past two weeks.
Public health experts also theorize that major LGBTQ Pride gatherings in June may have facilitated transmission of the virus. And given the infection’s incubation period — the new paper puts it at seven days, with a range of three to 20 days — the nation is now possibly seeing the resulting downstream effects of sexual encounters in late June and early July.
For the new study, a consortium of scores of researchers pooled data on 528 cases of monkeypox that were diagnosed between April 27 and June 24 at 43 sites in 16 countries. These cases included 84 people (16%) in the Americas and 444 (84%) in Europe, Israel and Australia.
All the cases were among men, including one transgender man, 98% of whom identified as gay or bisexual. This stark demographic finding is in keeping with data on the outbreak from around the world, such as a recent report from the British Health Security Agency finding that of the 699 monkeypox cases for which there was available information, 97% were in gay, bisexual or other men who have sex with men. New York City, the U.S. epicenter, has seen only one woman diagnosed with the virus out of 639 cases confirmed through July 19.
Accordingly, the European Centre for Disease Prevention and Control has characterized the risk of monkeypox to the general public, in particular those not engaging in sex with multiple partners, as “very low.” In a recent meeting, Dr. Agam Rao, a medical officer in the CDC’s Division of High Consequence Pathogens and Pathology, used the same words to characterize the general public’s risk.
In the new global study, the men had a median age of 38 and ranged between 18 and 68 years old. Three quarters are white, and 41% have HIV.
Despite some public health officials, including those at the CDC, cautioning the public about the risk of household transmission of monkeypox, just three of the 528 cases, or 0.6%, were believed to have been acquired through such means. And just four, or 0.8%, were considered to have transmitted through nonsexual close contact.
The study authors reported that 95% of the cases were likely transmitted through sexual close contact. What’s more, their paper offers strong new evidence that anal sex itself, although not necessarily ejaculation, is a major source of transmission.
“The strong likelihood of sexual transmission was supported by the findings of primary genital, anal, and oral mucosal lesions, which may represent the inoculation site,” the study authors wrote.
“The finding that 95% of cases may have been transmitted during sex provides reassurance that this outbreak is primarily caused by very close contact and may explain why it’s been largely limited, so far, to dense social networks of men who have sex with men,” said Dr. Jay K. Varma, an infectious disease expert at Weill Cornell Medicine.

Atypical to what has generally been seen in monkeypox cases in the 11 African nations where the virus has become endemic since it was first discovered in humans in 1970, people contracting monkeypox during this outbreak often have their initial development of lesions in the anorectal or genital area.
Nearly three-quarters of the men in the new study had lesions in those areas.
“It doesn’t seem like respiratory droplets or sprays have been an important mechanism of transmission, because if that were the case, you probably should have seen more cases among cisgender women. And by now, we haven’t,” said Dr. Céline Gounder, senior fellow and editor at large for public health for Kaiser Health News. “We also haven’t seen any evidence that monkeypox is transmitted through, say, hugging. So it really does seem to require pretty close, intimate contact to be transmitted.”
The World Health Organization recently reported that the monkeypox outbreak “continues to primarily affect men who have sex with men who have reported recent sex with new or multiple partners.” The CDC has recommended the Jynneos vaccine for men who report more than four male sexual partners within the past 14 days.
The new paper supports these characterizations of the outbreak. This includes its finding that of the nearly three-quarters of men who provided a sexual history, the median number of sexual partners they reported during the previous three months was five, with one quarter of the men reporting 15 or more.
During the previous month, 1 in 5 of the men reported they had taken drugs during sex, and one-third had sex at a sex-on-site venue. Of those who received testing, 29 percent had a sexually transmitted infection, or STI.
Public health experts have cautioned that monkeypox symptoms are often confused for STIs.
The new paper addressed the still open question of whether monkeypox might transmit through semen. Of 32 men’s semen analyzed, 29 samples had viral DNA present. Previous research has reached a similar conclusion.
Scientists note these findings do not confirm that semen transmits the virus. More research is needed, they say.
Some health authorities, including in the United Kingdom, have advised men who have recovered from monkeypox to wear a condom during sex for eight weeks as a precaution, should the virus remain in semen.
Condom use among gay and bisexual men has steadily declined since HIV became a treatable infection in 1996. The advent over the past decade of the HIV prevention pill along with scientific proof that treating HIV prevents transmission has hastened that decline. In a CDC survey published in 2017, nearly three-quarters of gay and bisexual respondents reported condomless sex during the previous 12 months.
Based on the new paper, Gounder said, “if you want to avoid getting monkeypox, and based on what we know about how monkeypox is transmitted, condoms will be very effective in preventing a bulk of or a majority of the transmission that we’re seeing right now and will be especially effective in preventing those most painful lesions.”
Monkeypox often prompts initial flu-like symptoms before a rash breaks out, followed by the emergence of skin lesions. In the new paper’s cohort, those initial symptoms most commonly included fever, exhaustion, muscle pain and headache. Thirteen percent of the men were hospitalized, most commonly for severe pain, in particular anorectal pain.
Even considering these hospitalizations, the study authors said, the health outcomes of the men in the study were “reassuring,” noting that the majority of cases involved no serious health complications.
Having HIV was not associated with any differences in monkeypox health outcomes. Because nearly all of the HIV-positive men were on successful treatment for that virus, they typically had healthy immune systems.
Dr. Chloe Orkin, an infectious disease expert at Queen Mary University of London and the lead author of the study, joined her colleagues in calling for greater awareness among health care providers of the manifestations of monkeypox in hopes of improving detection of cases.
Pointing to the paper’s many published images of how the virus can manifest at various sites on the body, as well as in the mouth and throat, she said, “We hope that doctors in primary care and emergency departments who don’t see many cases will also be able to recognize the many presentations and won’t miss the diagnosis.”