The first time I thought, I’d really like to talk to Demetre Daskalakis, was nearly 10 years ago. I’d read about the work he was doing in the newspaper. A reporter followed him around an afterhours gay sex club in New York City called Paddles. It was 4 in the morning, and he was there to give men meningitis vaccines. “That was an exciting, not much sleep time,” Daskalakis now says of the experience.
Back then, bacterial meningitis was tearing through the gay community in New York. A handful of people had died in the outbreak. Daskalakis didn’t have an official role; he was just an attending physician at a public hospital. Regardless, “Dr. Demetre” was becoming a familiar face at New York’s bathhouses and leather clubs.
Advertisement
Advertisement
Advertisement
Advertisement
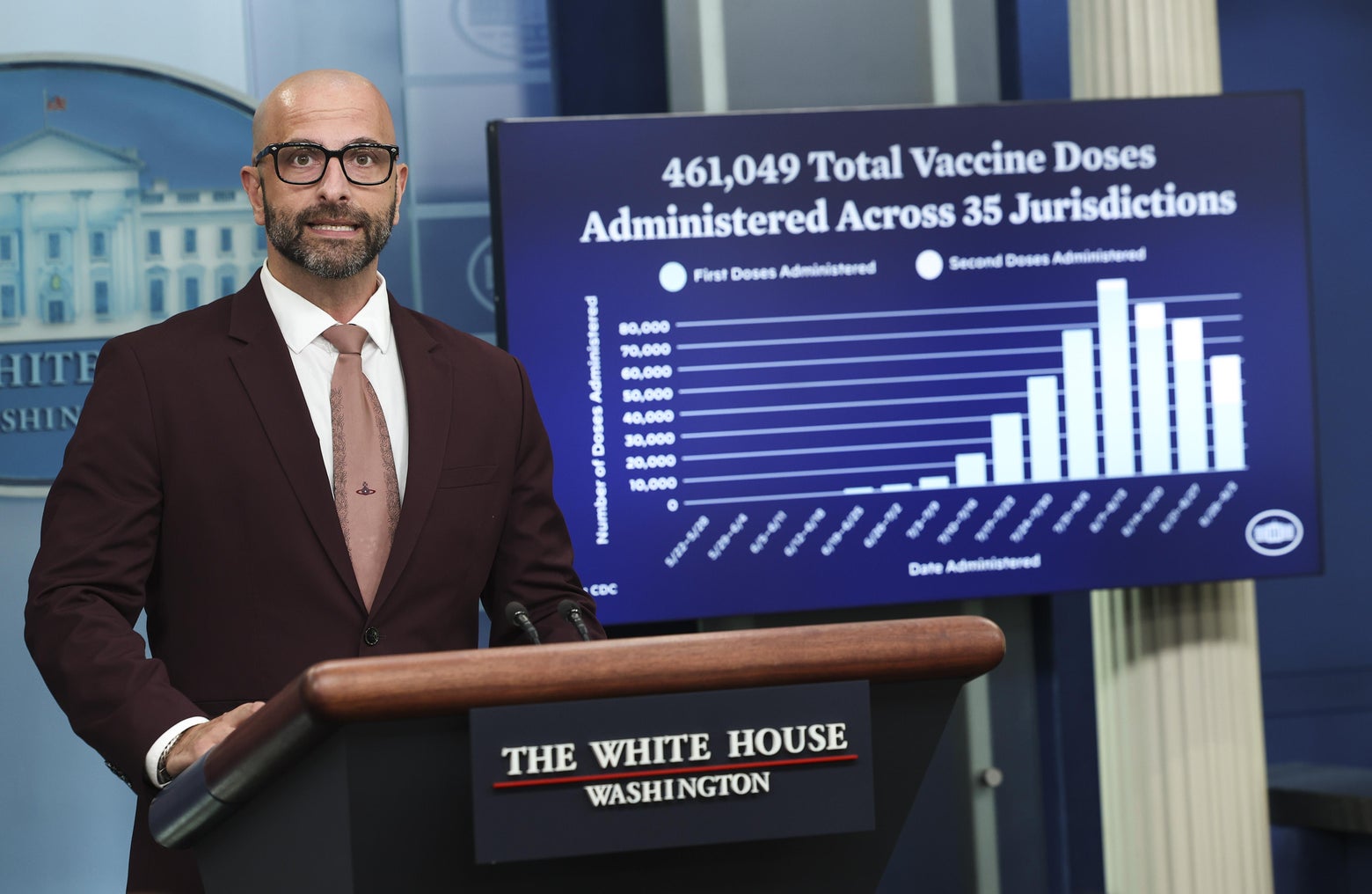
After the meningitis outbreak subsided, Daskalakis went on to lead HIV/AIDS prevention for the city health department. Fast forward to today, and his work has taken him all the way up to the White House, which is where he’s helping to lead the Biden administration’s fight against monkeypox as the deputy coordinator for the White House response.
The Biden administration has gotten plenty of criticism for being slow to respond to monkeypox. On Thursday’s episode of the show, Dr. Demetre Daskalakis explains why he thinks his radically open approach might be part of turning the tide.
Mary Harris: Demetre Daskalakis has been doing a lot of learning in real time about monkeypox. Before this outbreak, he was the director of the Division of HIV Prevention at the Centers for Disease Control and Prevention. His new role makes sense because this new strain of monkeypox, 90 percent of the time, is showing up in one group of people: gay men.
Advertisement
Advertisement
Demetre Daskalakis: It’s unprecedented. This is not the monkeypox that we are taught about in our infectious disease fellowship—a zoonotic disease that passes from animals to humans.
That’s not really the disease you’re looking at right now.
Advertisement
This is acting a lot differently, and it’s in a completely different social network. So it really calls upon not only the tools and the kit that you have for monkeypox, but also the tools and the kit that you have for infections that are associated with sexual activity and also the communities that are affected. Everyone had to brush up. We have fabulous pox experts at the CDC. And they were really important to us all getting up to speed, but then, everyone had to pivot because this outbreak is unprecedented and the way that it was moving in the population was unlike anything that we had learned or seen.
Advertisement
Advertisement
Advertisement
It’s funny because early on, in May, the administration was projecting confidence about their response to monkeypox. I wonder if you, with all of your knowledge of how some things spread in the gay community and the stigma and how that plays into treatment, were maybe a little bit more on edge about where this could go?
I feel like at that point I was more grateful that I was involved than on edge, because we were all working off of the monkeypox playbook: You have an exposure, you do vaccination of the exposed folks, and it’s controlled. When we saw that that’s not the story here, there was a pivot that the response took to reconsider their vaccination strategy, which was ring vaccination.
Advertisement
Advertisement
Advertisement
Advertisement
“Ring” vaccination—vaccinating an infected person’s close contacts—can stop a virus in its tracks, if you work fast. But over the course of June, as Pride celebrations played out around the country, it became clear this virus was moving faster than public health workers anticipated. Daskalakis says he got a fuller picture once the epidemiological data started coming in.
It took the epidemiology to teach us that this was moving a lot differently. This is a story that is characterized by a lot of pivots. So every time we learned something new, there was a pivot made to address it. And one of the most important pivots has been increasing vaccine supply to be able to be more broad in terms of the folks that we’re vaccinating.
Advertisement
In the midst of all this, I wonder how you’ve balanced your role as a queer health warrior and a government official. Over the summer, there was vigorous debate about whether people like you should be telling the gay community: “Listen, you should limit partners because while monkeypox is not a ‘sexually transmitted disease,’ it’s transmitted by close contact, and it’s spreading vigorously in this community.”
Advertisement
And you took a middle path. You said, “I think people should abstain from too many sexual partners, but this isn’t a forever thing.” And obviously you have your own kind of cred in the community. Can you talk about balancing all that? Because it seems like a tightrope.
Advertisement
It is a tightrope, but it’s the tightrope that I balance every day with HIV, so it’s super familiar. What we know from the story of HIV is that—and again monkeypox is totally different than HIV, but some of the story is very similar—you need to give folks harm reduction strategies that work for them, because there’s a whole range of humans in terms of what they’re going to listen to. Your folks who are very conservative sexually, you barely need to reach them. Folks who are in the middle, they’re swayable. And folks who are having a lot of sex, if you’re able to even address or change their behavior a bit, you’re gonna get some benefit.
Advertisement
And as the data increased over time, we also became stronger about being clear that the best strategy right now, while we’re waiting for adequate vaccine supply in the U.S. and folks to be vaccinated, is to reduce multiple partners or onetime partners in anonymous contexts. I’m not sure if you’ve seen the CDC guidance on safer sex and social gatherings, but it’s a pretty frank document that uses language that’s pretty clear. And that’s not the common way that public health has traditionally communicated to gay, bisexual men, and men who have sex with men, so that is really important.
Advertisement
Advertisement
With those guidelines, were you specifically like, “I don’t wanna use straight language here. I don’t wanna sound like a prude.”
Advertisement
Advertisement
Advertisement
That’s on brand. So I definitely wanted to make sure that the language was really frank.
Give me an example.
We used very clear terminology. So we didn’t shy away from talking about sex toys and fetish here and all of the things that we wanna make sure that people understand. We talked to community. We kept getting feedback. It was iterative. I often refer back to a document that inspired the safer sex guidance that I put out when I was in the New York City Department of Health for COVID. It’s all inspired by a document that’s called, I think, “How to Have Sex During an Epidemic: One Approach.” And it was community-driven.
Advertisement
“How to Have Sex in an Epidemic: One Approach” was a guide to safe sex that came out in 1983, when HIV/AIDS was spreading all over New York. It was published independently by a group of activists using donations. The guide gave information about the virus and recommended its readers use condoms and stick to certain lower-risk sex acts.
Advertisement
It’s a very frank, very clear document. And I remember when we were sitting in the office during COVID saying, “Gee, we really need to do this in New York City. We really need to make a document that leads and tells people strategies to prevent COVID in more intimate encounters.” And so we did, and it was really based on that. And so flash forward to monkeypox, and it’s pulling that idea out of the same toolkit and saying that public health needs to lead with this because we’re gonna be able to give people guidance that is correct based on science and nonstigmatizing.
Advertisement
I want to talk about where we are now with monkeypox. There’s some good news, right? Like the number of monkeypox diagnoses are on the decline as of this month?
Advertisement
Yeah. So looking at monkeypox, though we’re still seeing cases, we’re seeing a deceleration of new cases. It’s not consistent across the country. There’s some jurisdictions that are definitely decelerating, and they tend to be the jurisdictions that were earliest in the outbreak.
New York, Los Angeles?
Yeah, New York, Illinois, California—places where you had the initial outbreaks.
Advertisement
Advertisement
But the U.S. has still got a really high case count, right? Like more than 20,000 cases? And just for context, there are 55,000 cases globally. It’s a healthy chunk.
Advertisement
So we’re over 20,000, but what we’re seeing is that the doubling time of the outbreak is increasing, which means that it’s taking longer to double the number of cases. So it used to be in July, it took eight days to double the cases. And now we’re at over 25 days to double the cases.
We’re flattening the curve.
We’re flattening the curve.
Can I ask you to do something that’s gonna be hard for you, because I hear the optimism in your voice? What honest grade would you give to the administration for its monkeypox response so far?
I think that I have to give them a solid A.
Really?
Advertisement
I would, because this is unprecedented. I’ve worked on this since May, when I was at the CDC. And I saw the urgency with which people were moving with some of the challenges that were just seemingly insurmountable, and I’ve seen them being overcome.
Advertisement
But you started to say they’re unprecedented. And I think that’s why people have gotten stuck and sometimes angry about the administration’s response to monkeypox, because obviously we just had COVID, so people feel like with monkeypox we’ve seen some of the same challenges we had with COVID, where in the beginning, it was really hard to get a monkeypox test. And then it was really hard to get a monkeypox vaccine. And then when the vaccines were out there, there were long lines and there were people gaming the digital system. This is what happened in New York City; that’s where I am. People had real questions about whether the right people were getting treatment. And so it felt like a retread, and as someone who follows public health closely, I was frustrated. And I can’t imagine you weren’t.
Advertisement
Advertisement
I’ll say I’ve been in a lot of responses. And every response feels like it needs to go faster, and that’s always true because it’s an emergency. But if you actually look back at this one and look at the speed at which some things happened, it really demonstrates that some of the lessons and strategies from COVID were actually working. So, the time from when the first case happened—a week later, CDC was already talking to commercial labs to get the lab commercialized. Within a month those labs were commercialized and available for doctors to order routine mechanisms. That’s unprecedented. The speed of going from a test that was in a public health lab all the way to commercialization, that’s a direct lesson from COVID that moved really quickly.
Advertisement
Advertisement
Advertisement
The vaccine! So this is a vaccine that’s stored in the Strategic National Stockpile. No one imagined using a bioterrorist-preventing vaccine as a strategy to address an infection that was moving through close skin-to-skin contact in the context of sexual activity. And so the system had to pivot.
I wonder if it gave the administration a false sense of security, like, Oh, we got this. This is in the stockpile. So, we’re good.
I don’t think anyone had a false sense of security. From where I sat at CDC, and then now where I sit at the White House, I feel like everyone’s aware that the challenges are real. And just, the creativity with which those challenges have been addressed has been remarkable as has the speed.
Advertisement
I feel like what you’re saying is like the COVID response was probably frustrating, and all those frustrating things may have happened this time, but we got past them faster.
Advertisement
That’s probably a great summary. COVID taught so many lessons, and one of those was onboarding and testing faster. Everyone wants everything to move faster, and they’re right: It’s an emergency. But I was amazed at the speed with which commercialization of a labs happen.
Advertisement
Can you get the genie back in the bottle? Do you think we can eliminate monkeypox at this point, or is it too late in the U.S.?
I think that we are on the way to really tight control of this outbreak.
Advertisement
That doesn’t sound like elimination.
Well, my next sentence is then we have to really also focus, not only domestically, but also internationally. And that’s gonna be a really important focus of the work that we’re doing, because there’s always the possibility of reintroduction. I would love to shoot for elimination. Today I’m gonna take really tight control.
I think the major challenge right now is vaccine distribution. You’ve talked about it a couple of different times in a couple of different ways. Last month, you and others in the administration made a decision that some saw as controversial, which was to split up the dose of the monkeypox vaccine into five doses and give it slightly differently—under the skin, as opposed to inside the body. This may be a dumb question, but why can we just not get more vaccine?
Advertisement
That’s not a dumb question. It’s actually a great question. It’s all about the when and the how. First of all, the intradermal strategy, given the data that we have, and the very thorough review done by the FDA, that strategy is a really important one to expand what we already have on the ground.
Advertisement
Advertisement
But this plan has been criticized. In the Washington Post, Dan Diamond and some other folks reported that the day after the FDA started exploring this idea of splitting up the doses, the manufacturer called and they were hopping mad, threatening to cut off all future vaccine orders to the U.S. because they said we don’t know how workable this is. That seems bad.
Advertisement
Advertisement
We’ve reviewed their data thoroughly along with them. And I think one of their issues was around safety. We actually did look at one of the studies using the vaccine virus that’s used; 7,000 people were vaccinated in Germany with the same vector, with great amounts of safety. So there’s definitely interactions that happened with the company, but ultimately everyone right now is on the same page.
Not everyone is on the same page, of course. Earlier this month, infectious disease researchers at Erasmus Medical Center in Norway released data that raised real questions about the plan to shrink vaccine doses. It suggested the shots weren’t generating many antibodies in people who got them.
Daskalakis says this new information doesn’t change his thinking that much—yet. That’s because the Erasmus study looked at intramuscular injections rather than the intradermal injections his team is recommending.
Advertisement
Advertisement
It’s kind of like apples and sawdust. We’re not really able to compare it to the intradermal. The next part of this is gonna be that we are also gonna be conducting vaccine effectiveness work across the country, and we’ll be looking at various dosing strategies with real-world monkeypox challenge.
Do you feel like part of your challenge as a public health communicator with outbreaks like this is finding a way to reassure people while also acknowledging that what’s going to happen over the next six months or year is going to be by definition an experiment?
Yeah, this is the really important part about communication in any outbreak, which is that what we know today could be different tomorrow. And that’s not just about outbreaks, but about everything that we do because we move with the science. So, the science will teach us new things. And we’ve got to be ready to express how the changes are happening.
Subscribe to What Next on Apple Podcasts
Get more news from Mary Harris every weekday.







