When infectious diseases physician Dr Jonathan Volk learnt about monkeypox at medical school in the United States more than a decade ago, he was taught it was a mild, self-limiting illness.
In the past few months, he’s diagnosed nearly 160 cases at the Kaiser Permanente San Francisco medical centre. Most have been mild, but some have not.
“Many patients have had excruciating and difficult-to-control pain, including severe rectal pain and bleeding,” Volk says.
Some have painful mouth lesions that make it difficult for them to eat, others have severe itching, and some develop secondary bacterial infections in the virally caused lesions that are characteristic of the disease. None so far have been hospitalised.
Last month, the World Health Organization said the spread of monkeypox to 75 countries and territories warranted its elevation to a public health emergency of international concern, with the aim of encouraging global co-operation to address the disease. More than 36,400 infections have now been recorded throughout the world. Australia has reported 82 cases so far, mostly in New South Wales and Victoria. WHO notes that monkeypox is not as contagious as some other infections, because it requires close contact to spread. In his announcement, WHO director-general Tedros Adhanom Ghebreyesus commented that, so far, the outbreak was concentrated among men who have sex with men and highlighted that “stigma and discrimination can be as dangerous as any virus”.
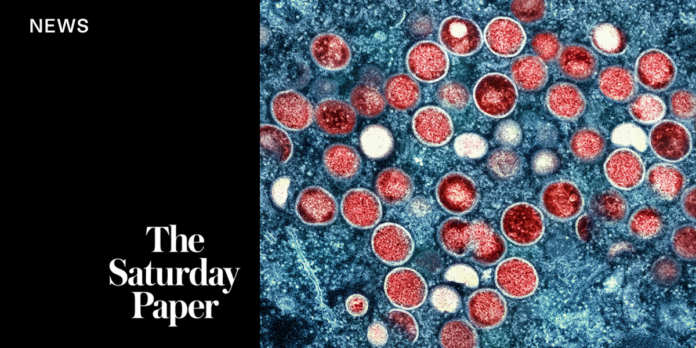
Like SARS-CoV-2 – the virus that causes Covid-19 – monkeypox is a zoonotic virus, meaning it can transmit from animals to humans. Monkeypox was first identified among monkeys kept for research in 1958 – hence the name – but the disease infects rodents as well as primates, and one human case in the US in 2003 was even linked to an infected prairie dog. The first human case was recorded in 1970 in a nine-month-old baby in what’s now known as the Democratic Republic of Congo. Since then, there have been sporadic outbreaks in central and west Africa, with occasional cases reported outside that region in travellers from the area or in people who encountered infected animals. However, since 2017, Nigeria has been in the grip of a much larger outbreak that has infected an estimated 700 people.
The disease commonly starts with a fever, swollen lymph nodes, headaches, muscle aches and exhaustion. Within a few days of that prodromal stage, the distinctive “pox” appear – small bumps that become pustular, then crust over and eventually heal. Prior to the current outbreak, these lesions were mainly thought to appear on the face, hands and feet, and inside the mouth. But in this latest outbreak, most have developed lesions in their genital region, something previously only reported in about 30 per cent of cases. The course of infection lasts about two to four weeks. The case fatality rate in previous outbreaks in Africa has ranged from about 3.6–10.6 per cent, and five deaths have so far been reported outside Africa in this outbreak.
The timing of the Nigerian and global outbreaks is unlikely to be a coincidence, says Professor Andrew Grulich, an epidemiologist and public health expert at the Kirby Institute at UNSW Sydney.
Monkeypox is one of the orthopox group of viruses, which includes the pathogen that causes smallpox, an infectious disease long since eradicated by vaccines but one that is still the stuff of nightmares for those working in infectious diseases and public health. The global smallpox vaccination campaign, considered one of the great public health success stories, had largely wrapped up by the 1980s. “It means young people today pretty much nowhere are vaccinated against smallpox,” Grulich says.
Another temporal factor in this outbreak may be its emergence during the northern hemisphere summer, he says, “when all those massive gay Pride celebrations were happening for the first time in three years, so were probably more joyous than normal. It gave this bug fertile ground to spread.”
Mindful of the dark history of early HIV/AIDS coverage that implied the disease was a “gay plague” and led to widespread vilification and stigmatisation of those suffering from it, public health groups in Australia are working closely with the LGBTQIA+ community and health organisations to ensure the messages around testing, treatment and vaccination get to the right people and in the right way.
Public health sociologist Jennifer Power stresses the importance of “sex-positive” messaging around monkeypox. “I always use the example of the community-based HIV response, where it was very deliberately almost celebrating the sex cultures among gay men, like their sexual sociability, or sex-based sociality,” says Power, who is an associate professor at the Australian Research Centre in Sex, Health and Society at La Trobe University.
“[It] is really just acknowledging that sex has been part of queer culture, part of gay men’s culture, for the sake of sex and pleasure, but also social networks and connecting and being part of community.”
Power says there’s a risk during a public health crisis that the need for human social connection is disregarded, “like we’re all meant to suddenly become these very rational humans who make decisions about how we love or who we have sex with in these black-and-white, rationalised terms,” she says. “It’s just not how humans work.”
The Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) and the Australian Federation of AIDS Organisations have joined forces to help shape and co-ordinate the response to monkeypox. This partnership approach, also involving researchers, clinicians and community, has proved extremely successful in dealing with HIV/AIDS and other diseases that have disproportionately affected the gay and bisexual community, says ASHM president Dr Nick Medland, a clinical epidemiologist also at the Kirby Institute.
“A characteristic feature of the Australian HIV/AIDS response is the way that the health workforce – not just doctors and nurses, but also researchers and laboratory science – work together with the affected communities to make sure that we’re all singing from the same song sheet, and that the approaches to these outbreaks, these epidemics, is consistent and it’s focused on the people who are most affected by them,” he says.
But exactly what those approaches are is still being worked out, largely because the vaccines that can prevent infection – both before and just after exposure – have limited availability in Australia. “The message can’t be ‘get vaccinated’ if we haven’t got enough vaccines yet,” Medland says.
Two smallpox vaccines – ACAM2000 and JYNNEOS – have been approved against monkeypox. The former is more available, as part of the Australian government’s existing vaccine stockpile in case of smallpox outbreaks, but it can’t be used in people with compromised immune systems. It also requires special training to administer and is associated with rare but potentially serious side effects. Shipments of JYNNEOS, which is less associated with side effects and can be used in immunocompromised or pregnant people, have recently arrived in Australia, but the quantities are still relatively small.
The federal Department of Health has recommended vaccination for men who have sex with men and who have recently had a high number of sexual contacts, have attended sex-on-premises venues or had group sex. It’s also recommended for high-risk contacts, sex workers and anyone planning to travel to a country with high levels of risk.
The infection can also be treated with antivirals, but Grulich said these are not readily available and tend to be reserved for people hospitalised with severe disease. Some also require pain relief, as severe infection affecting the rectum can cause extreme pain.
For the majority of those affected, all they can do is self-isolate and wait for the lesions to heal. As the Covid-19 pandemic has revealed, that is far from easy, and Volk stresses the need to acknowledge the challenges of this and support those affected. “It has been critical that we address the stigma, mental health and economic consequences of asking patients to isolate for weeks,” he says.
This article was first published in the print edition of The Saturday Paper on
August 20, 2022 as “Lessons for monkeypox”.
A free press is one you pay for. Now is the time to subscribe.