Even before the Affordable Care Act reduced uninsured rates in our country, it required private insurers to cover essential preventive care at no cost to patients. But just as other pieces of the law require enforcement, so does this one.
Today, many individuals face obstacles to accessing affordable treatments that prevent HIV despite insurers’ legal obligation to provide them and federal guidance requiring they be made freely available. In the fight to end the HIV epidemic, federal and state regulators must hold noncompliant health plans accountable to ensure that people can receive the medication and services they need to prevent HIV.
advertisement
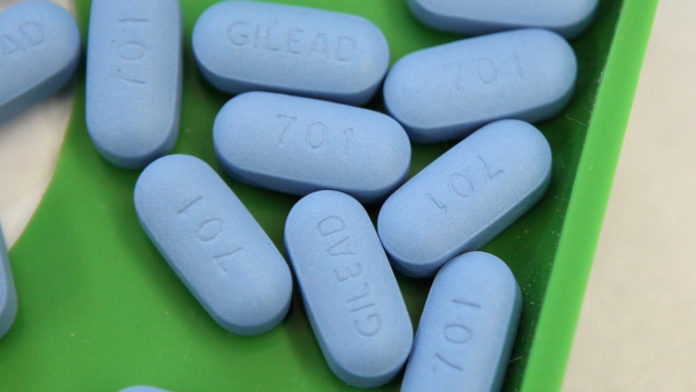
Pre-exposure prophylaxis, known as PrEP, is a highly effective medication that can prevent HIV from sex or injection drug use. When taken as prescribed, PrEP reduces the risk of HIV infection through sex by 99%, and by 74% among people who inject drugs. In 2019, the U.S. Preventive Services Task Force (USPSTF) gave PrEP an “A” grade, meaning it recommends the measure and has high certainty that its offers substantial benefit. The task force recommends that providers offer PrEP to people who are at high risk of contracting HIV.
Based on the A grade recommendation, almost all private health plans were required to provide PrEP at no cost to patients beginning in January 2021. That decision was an important milestone, because the Affordable Care Act requires private insurers to offer services with “A” or “B” grades without patient cost sharing, meaning they face no copays, coinsurance, or deductible payments for PrEP.
advertisement
Yet less than one in five individuals who are recommended to take PrEP are receiving the medication today. Its uptake has traditionally been slow among populations at higher risk of HIV, including Black and Latino gay men and Black women.
Without proper enforcement, some private ACA health plans across the country have violated the legal coverage requirement for PrEP, limiting its use by individuals who want to protect themselves from HIV. In July 2021, my organization, the HIV+Hepatitis Policy Institute, updated a report showing that several plans were still in violation of the ACA requirement for PrEP coverage, even seven months after the January 2021 deadline for almost all plans to comply under the USPSTF recommendation for covering the medication.
The federal government and state insurance regulators are responsible for reviewing compliance with this requirement and must step in to ensure that insurers are following the law. Their compliance should be reviewed on a recurring basis — potentially every three months — and those that deny or limit access to PrEP should be penalized. Lack of timely enforcement and penalties puts people at risk of contracting and spreading HIV, which is completely at odds with the dedicated public health efforts to end this epidemic.
Private insurance plans in several states have attempted to limit PrEP access by placing the medication on higher insurance coverage tiers that increase patients’ out-of-pocket costs or by requiring them to try less-expensive versions of the drug before covering the medication prescribed by their doctor, a process often referred to as step therapy.
To provide clarity on how private ACA plans should cover PrEP and related services, the federal government released in July new frequently asked questions (FAQs) on the USPSTF recommendations for HIV-prevention drugs. The FAQs reinforce patients’ access to PrEP treatment and PrEP-related services such as screening tests for HIV and sexually transmitted infections at no out-of-pocket cost. The FAQS also emphasize that treatment decisions about PrEP should remain between a patient and their provider — not the insurance company — and clarify that plans must provide an easy exemption process for patients who may experience roadblocks in accessing the medication because an insurer used burdensome practices to limit access to the drug, such as step therapy. Any PrEP drug a provider approves for a patient through the exceptions process must also be available at no cost. This critical guidance builds on existing patient protections and will help reduce barriers to PrEP for patients.
But regulators, patient and provider advocates, and all HIV stakeholders shouldn’t stop there. The USPSTF recommendation and subsequent federal guidance must be fully publicized to patients and enforced across private ACA health plans. It’s essential that patients and their providers understand their rights to receive PrEP for free and know they have the power to file complaints with their insurance plans and state insurance commissioners if they face access barriers to accessing this medication.
The new federal FAQS that clearly explain patient coverage requirements for PrEP empower communities with another tool to protect people from HIV and advance health equity. But there needs to be a unified commitment among federal and state regulators and the HIV community to make it as easy as possible for people to know that PrEP and its associated services are available without cost-sharing.
If federal and state regulators don’t hold plans accountable for covering PrEP, people at risk of HIV will continue to face unnecessary financial and coverage barriers to a treatment that can help eliminate a deadly virus. The clock is ticking: While plans must offer PrEP without cost-sharing now, private plans and insurers have until September 17, 2021, to comply with all other aspects of the updated FDA guidance.
Carl Schmid is executive director of the HIV+Hepatitis Policy Institute, which promotes quality and affordable health care for people living with or at risk of HIV, hepatitis, or other serious and chronic health conditions. The HIV+Hepatitis Policy Institute receives funding from several pharmaceutical companies, including Gilead and Merck, who have or may have PrEP products now and in the future.