Since his two-year-old son’s routine blood test in November showed the child had been lead poisoned, Charrell Reed and his family have felt like prisoners in their apartment on the city’s West Side.
Reed, 27, who works as a subcontractor for a home renovation company, knows how dangerous lead can be. He and his sister were poisoned as children, and their uncle, Darrick Wade, has been crusading against the toxin since his son, Demetrius, was exposed in public housing in the 1980s and died at age 24.
Using his uncle’s connections, Reed was able to get a lead expert to test the paint in the apartment, confirming his suspicion that the heavy metal, which can cause irreversible neurological and other health effects, was there.
And yet, Reed says he feels stuck. Even though he knows the lead is there, he hasn’t been able to get any help cleaning it up from his landlord or city health officials—partially because of the pandemic.
 Charrell Reed The pandemic has made diagnosing lead poisoning and fixing hazards in homes even more difficult than it’s always been, as families are skipping pediatric appointments out of fear, and some lead inspectors and short-staffed health departments have had to delay or halt in-home work.
Charrell Reed The pandemic has made diagnosing lead poisoning and fixing hazards in homes even more difficult than it’s always been, as families are skipping pediatric appointments out of fear, and some lead inspectors and short-staffed health departments have had to delay or halt in-home work.
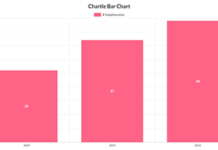
In the first five months of 2020, 34% fewer children in the United States were tested for lead levels than in the same period in 2019, according to the Centers for Disease Control and Prevention (CDC). in Ohio, 51% fewer children were tested for blood lead levels in May 2020 compared to May 2019.
Much of the drop has been attributed to people’s fears of being exposed to COVID-19, choosing instead to postpone routine doctor visits.
While testing began picking up again as pandemic restrictions eased, experts worry that many children fell through the cracks—either never getting tested, or, if they did, ending up on a list of backlogged cases for overtaxed health departments to inspect.
The pandemic made it harder for families to get their homes tested for lead, and to get the help they need to make repairs when a source of the poisoning is identified in the home—particularly during the first few months of the shutdown.
The CDC reported that local health departments across the country were struggling to conduct in-home lead investigations and other home visits due to staffing shortages and fears of exposure to the virus.
The city of Cleveland declined to comment on its lead poisoning prevention efforts during the pandemic.
For Reed’s family, and for many others in the same situation, the inability to get help from people qualified to clean up the lead in a safe way convinced Reed the family needs to move—as quickly as possible.
“If I can’t get [them] to work with me the correct way, then we’ll just leave [if] it’s going to be a continuing problem,” Reed says. “That’s the main task, just hit the road. If we can be up out of here tomorrow, we are going tomorrow.”
Trying to find help
Reed’s personal experience with lead poisoning made him very attentive to a potential problem: When he moved into his apartment last spring he repeatedly asked his landlord to fix the peeling paint he saw on the window sills. His pleas went unanswered.
Reed tried to keep his son away from the area, and got him tested for lead at his annual well visit, just as he had a year earlier and according to recommendations from health experts.
Yet despite his knowledge and initiative, Reed’s family still hasn’t received any help. Though he knows better—lead is impossible to see, and spreads throughout homes in tiny dust particles that are difficult to clean up completely—he still blames himself.
People like Reed are the reason Yvonka Hall helped co-found the Cleveland Lead Safe Network in 2016.
“In Cleveland about 90% of our homes are lead impacted,” Hall says. “And in our first-ring suburbs, it’s about 80%.” In 2019, roughly 1,000 children were poisoned by lead in Cuyahoga County, with another 750 in the city of Cleveland.
In Hall’s eyes, the solution to the reluctance to get children tested at the doctor’s office is to bring the testing closer to parents by having mobile testing stations travel to impacted neighborhoods. Hall says she believes the city can afford the service. “You got the money, do the work,” she says. “There’s no work being done.”
Mobile testing would begin to address the problem that Dr. Aparna Bole has seen throughout the pandemic—parents not bringing their babies and young children in for regular doctor’s appointments. As a pediatrician at University Hospitals Rainbow Center for Women and Children, Bole also is concerned that children have been inside the home more than usual, due to remote learning and other social isolation measures.
Exposure at such a young age can have lifetime neurological consequences that can manifest into lower academic performance, Bole says, and high lead levels have been linked to other health issues later in life—and even adult criminal behavior.
“The pandemic is exacerbating some of these housing-related exposures,” Bole says. “I see a lot of kids in very, very sub-optimal childcare situations because parents have no choice.”
Resources exist to help people once they find out their house has lead or that their child has high lead levels. More needs to be done, however, to prevent the lead exposure in the first place, “instead of testing the kid’s blood, finding out they’re poisoned, and then trying to address the problem,” she says.
A law passed in 2019 by the city of Cleveland requires all landlords to pay for private inspections and secure lead-safe certificates for their rental units. The law also requires additional disclosures to renters and homebuyers about whether a home has an identified lead hazard.
The new law went into effect on March 1 this year and is being gradually rolled out by zip code.
For now, a combination of education and in-home preventive measures is the next best way to reduce chances of exposure to lead.
As director of training and healthy homes for Environmental Health Watch, an environmental justice organization, Akbar Tyler sees firsthand the condition of homes where children have been spending all their time during the pandemic. Tyler conducts home inspections and teaches residents how to keep their kids safer when there is lead in the home.
The first line of defense, Tyler says, is to eliminate the most common sources of lead—flaking paint and dust. The second line of defense is to keep floors and other surfaces clean of dust, which can contain tiny particles of lead that are easily transferred from hand to mouth by babies and toddlers. The last line of defense is good nutrition—calcium- and iron-rich diets make it harder for bones, joints, and soft tissue to absorb lead during the 30 days or so that it stays in the blood.
“Eliminating the hazard in a safe way is the way to stop children from getting poisoned,” Tyler says.
The struggle of identifying the hazard of lead—through a blood test, a home inspection, or both—and figuring out what to do next, has been an effort than many parents can’t bear, especially during a pandemic. As people like Reed have discovered, community resources and health department interventions that should be available often don’t arrive until too late.
“A lot of parents, they blame themselves,” says Hall. “[They ask], ‘what could I have done to prevent this from happening to my child?’” Like Reed, the only thing that many families can do to immediately help their children is move, and hope to find a lead-free home, she says.
That’s exactly what Reed and his family plan to do, even if it means breaking the lease, because the longer they stay in their apartment, the more his son’s health is at risk, he says.
“When you have kids, you need to protect them every step of the way,” says Reed. “I just want to get up out of here immediately more than anything—Me, the wife, and the kids, go.”
Sardo-Longo, Tluang, Chau, and Gay are high school students at The School of One in Cleveland and North High School in Akron, Ohio. They were participants in Urban Health Media Project’s workshop, “Home Sick: How Where We Live Impacts Health” in Spring of 2021.