On June 5, 1981, the Centers for Disease Control and Prevention (CDC) released a report on a rare pneumonia and lung infection. One month later, a story in The New York Times with the headline “RARE CANCER SEEN IN 41 HOMOSEXUALS” detailed an illness striking gay men in New York and California.
Three years later, this “rare cancer” was officially diagnosed as Acquired Immunodeficiency Syndrome, a disease caused by a retrovirus that interferes with the body’s ability to fight off infections and disease. Panic was felt the world over as scientists raced to understand how the new infection, better known as HIV/AIDS, was spread and who was most at risk.
That same year, Anthony Fauci, a doctor and head of the Laboratory of Immunoregulation, was appointed as National Institute of Allergy and Infectious Disease (NIAID) director.
“In 1984, the virus was discovered, which set off a series of extraordinary research to determine the pathogenic mechanisms of HIV. But importantly, it allowed us to do the critical research to start developing effective drugs for HIV,” Fauci tells PopSci in a recent interview.
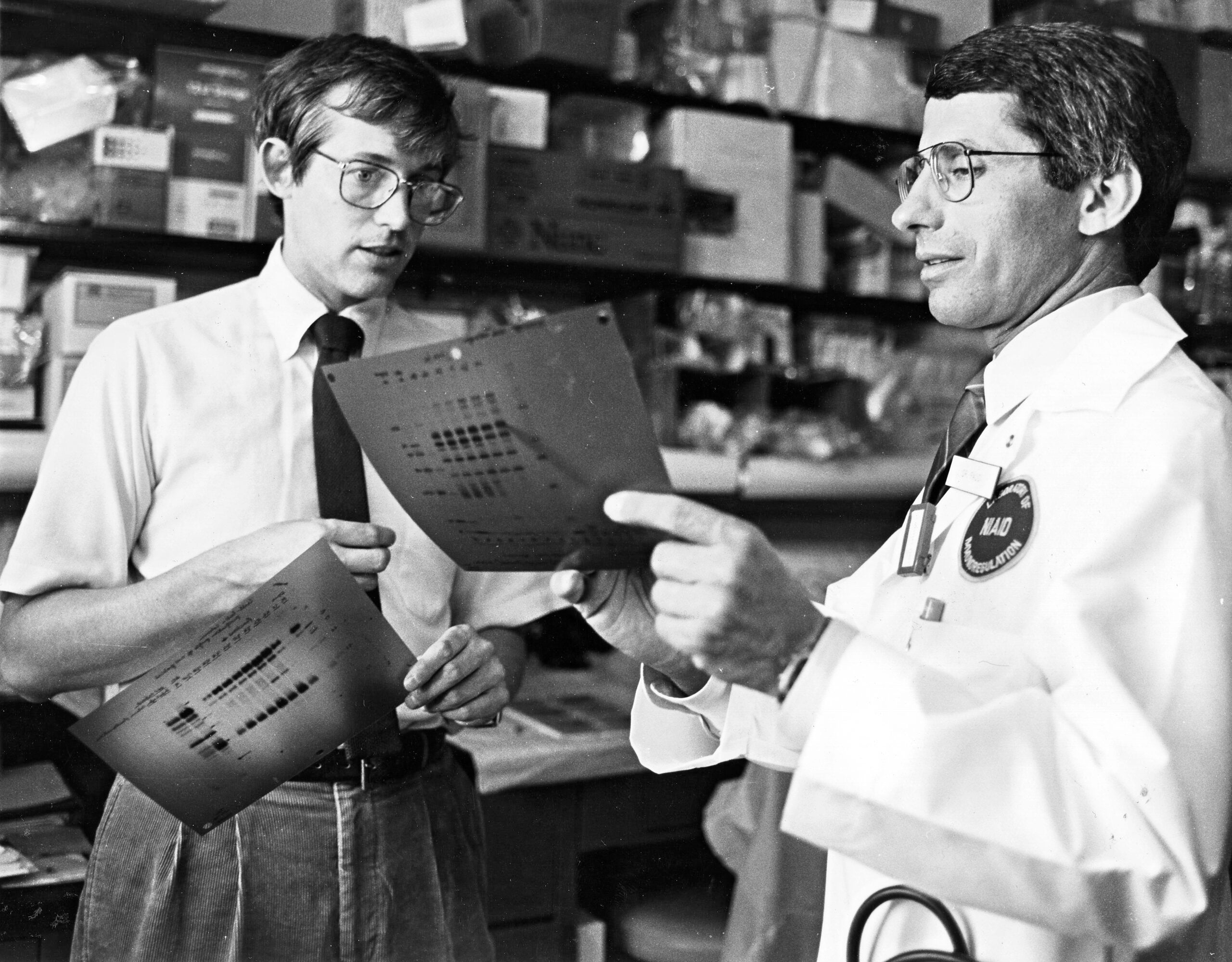
Office of NIH History and Stetten Museum
By the end of the 1980s, almost 700,000 people of all sexes and sexualities were estimated to be living with HIV. While knowledge on the virus and the disease has steadily progressed over the past 40 years, the fight against the epidemic continues globally.
According to World AIDS Day, an international awareness event celebrated annually on December 1, an estimated 38 million people now live with the virus worldwide. More than 35 million people have died of HIV/AIDS related illnesses since it was identified.
But Fauci, who has studied HIV/AIDS since the first cases emerged, finds hope in the treatments and advances over the last four decades that help patients to live longer lives. In 2003, he played an important role in developing the President’s Emergency Plan for AIDS Relief (PEPFAR), marking a pivotal point in government funding towards the global epidemic and a program he is proud to have been part of.
“That program has now been shown to be responsible for saving literally 20 million lives worldwide,” Fauci says.
[Related: Rare transplant cells have cured another HIV patient]
Despite scientific progress, however, unequal access to HIV/AIDS treatment has been difficult to solve, along with another obstacle that is less scientific and more social: the stigma that accompanies new diseases. As cases emerged, people with HIV/AIDS were often alienated, overlooked, and even loathed by the public. Discussions around sexual orientation, promiscuity, and individual behavior often centered the blame on the gay community and later, drug users, as these groups made up a large proportion of cases in the 1980s and 1990s. This negative connotation still prevents some people from seeking treatment.
“Stigma is the enemy of public health,” says Fauci. “There is no place [for] the stigma when you’re dealing with a disease, because it’s the disease [that] is the problem, not the people who are afflicted.” He and the National Institute of Health were even the direct targets of protests by AIDS Coalition to Unleash Power in 1990. The organization formally called for Fauci to include their members in the development of HIV drugs.

The stigma of disease—often attributed to minority groups—persists today. For those who remember the early days of the HIV/AIDS crisis, this year’s global monkeypox outbreak seemed to mirror the prejudice toward the gay community in the late 20th century. Notably, during the COVID-19 pandemic, Asian communities were blamed for bringing the coronavirus to the US. Black, Indigenous, and Latinx Americans have also been disproportionately affected by the sickness.
As the infection took hold everywhere, Fauci needed to address stigma, while simultaneously sharing medical knowledge and pivoting to his role as the country’s most prominent health communicator.
“Given the circumstances of a historic pandemic, as a scientist and as a public health official, I felt [it] was necessary to step up to the level of trying to create policy that would get the best of the science available to the American public, as well as the messaging that [was] necessary to get the right public health interventions implement it,” he says.
Now, nearly three years after the first coronavirus cases, the stigma is being felt by those who suffer from long COVID. An estimated 16 million Americans—a number that could grow—are currently experiencing the debilitating condition.
[Related: The 5 phases of COVID’s endgame]
“I think from the beginning of the COVID pandemic, there’s been an ableist undertone,” Marija Pantelic, a lecturer at Brighton and Sussex Medical School in the UK, who studies stigma and disease, tells PopSci. “We were hearing so many testimonies [of long COVID], but there had been no work that I could find really, that empirically looked at the extent of this problem.”
Pantelic led a study published on November 23 in the journal PLOS One that found that the majority of people living with long COVID experience some form of stigma directly related to their condition. She and her colleagues surveyed more than 1,100 patients about their experiences of enacted stigma, internalized stigma, and anticipated stigma. They found that 95 percent of the adults in the UK who were surveyed experienced at least one type of stigma at least “sometimes,” and 76 percent experienced it “often” or “always.” Those numbers shocked Pantelic.
“I think a notable difference in the stigma is that long COVID is really psychologized, meaning that people are told that it’s all in their head,” she says. “Even a lot of healthcare providers dismiss it.”
According to Pantelic, raising awareness of diseases like HIV/AIDS and long COVID is often an important first step. Numerous groups like Long COVID Support and the Long COVID Alliance have emerged since the beginning of the pandemic, and have used platforms like social media to help mobilize efforts.
“It’s really essential to acknowledge the role of communities. And mobilizing, I think that is a key similarity between HIV and COVID,” Pantelic notes. “It would be lovely for us to learn from the HIV movement.”
“Stigma is the enemy of public health.”
Anthony Fauci, director of NIAID
But it can’t end with raising awareness: Keeping people safe requires hard, long-lasting work. Currently, public health organizations are working to correct the errors of the past, and the World Health Organization announced on Monday that it would change the name monkeypox to mpox in an effort to fight stigma and stereotypes.
For HIV/AIDS, action has led to treatments such as the daily antiretroviral therapy and the HIV prevention drug PrEP, which helps keep the virus at bay. Current treatments are primarily long-term “forever” pills, which may make the disease less deadly, but still allow it to persist as a chronic illness in patients.
[Related: The first people have received an experimental mRNA HIV vaccine]
“I think we’re going to get more user-friendly methodologies of treatments and long acting antivirals that can be given maybe every six months,” says Fauci. “That’s an amazing improvement rather than a single pill.” Further into the future is the hope that an HIV vaccine could change the course of the disease—and hopefully eradicate stigma.
After 54 years with the National Institute of Health, 38 years at NIAID, and seven presidential administrations, Fauci has faced stigma and scientific challenges head on—from HIV/AIDS, to Ebola, to Zika, to COVID. While he is stepping down from government service at the end of December, he plans to continue writing, lecturing, and working.
“I might be able to help the effort of public and global health,” he says, “and perhaps inspire and encourage young people to pursue a career in science, medicine, public health, and hopefully in a public service.”