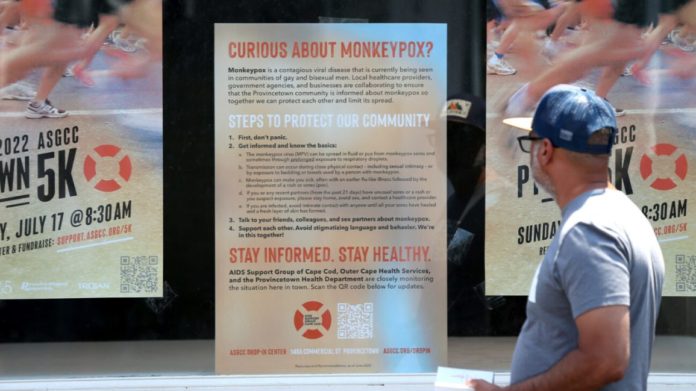
- A new survey by Annenberg Public Policy Center showed about 20% of people are concerned about getting monkeypox.
- The monkeypox virus is not new, and there’s a vaccine available. But many Americans are unsure or don’t believe that a vaccine exists.
- Monkeypox is a serious health issue, but it is typically not deadly. Still, experts say knowledge, caution, and vaccination, when applicable, are important.
News of a virus known as monkeypox began making headlines in the U.S. in May when the
On May 18th, the first U.S. case was confirmed in a man from Massachusetts.
More than two months later, two states — New York and California — declared states of emergency over the monkeypox outbreak.
The terminology can ring all too familiar — COVID-19 is still considered a global pandemic. Now, there’s another health issue to worry about, and 1 in 5 Americans are concerned about getting monkeypox, according to a national survey by Annenberg Public Policy Center.
It’s a lower rate than individuals who fear getting COVID (1 in 3), though 48% are not sure which of the two viruses is more contagious.
Annenberg found another issue with information about monkeypox: 66% are unsure or do not believe a vaccine for monkeypox exists.
Furthermore, misinformation and disinformation about monkeypox are spreading faster than the virus.
To help raise awareness and clear up misconceptions, we asked health experts to answer common questions most people have about monkeypox and how people can best protect themselves. Here’s what they had to say.
“Monkeypox is a viral infection stemming from the same family as the smallpox virus,” explains Dr. Thomas Yadegar, medical director of the intensive care unit at Providence Cedars-Sinai Tarzana Medical Center. “It is a self-limiting disease, meaning that as time progresses, the infection should resolve itself.”
Though people in the U.S. may just be learning about monkeypox, it is not a new virus.
“The monkeypox virus was first discovered in monkeys in 1958, and then in humans in the early 1970s,” says Rachel Cox, DNP, FNP-BC, an assistant professor in the School of Nursing at MGH Institute of Health Professions. “Although monkeypox and smallpox have similar symptoms, monkeypox is generally milder and much less likely to cause death.”
Cox says monkeypox symptoms include:
- rash
- fever
- chills
- body aches
- fatigue
- headache
- respiratory symptoms, such as a sore throat, cough, and nasal congestion
- swollen lymph nodes
Cox further says the rash may appear on the:
- face
- genitals
- mouth
- hands
- feet
- chest
- anus
“The rash often begins with flat lesions that become raised, similar to blisters or pimples, and then fill with fluid and pus,” Cox says. While the rash is present, the skin may be very sensitive and painful. “The blisters usually scab or become crusty and then fall off, potentially leaving scars on the skin.”
Currently, most monkeypox cases are in men who have sex with other men. Still, Dr. Michael Chang, a pediatric infectious disease specialist at Memorial Hermann in Houston, stresses that no one is immune to monkeypox infection. It does not care about your sexual orientation, age, or health status.
“Monkeypox can spread to anyone — children and adults, healthy or immunocompromised,” Chang says.
Chang says the primary mode of transmission is skin-to-skin contact. This contact may include:
- direct contact with monkeypox rash, scabs, or body fluids, including respiratory secretions from a person with monkeypox
- close or direct contact, usually defined as sexual activity, hugging, kissing, or prolonged face-to-face contact
- touching unwashed objects, fabrics (clothing, bedding, or towels), and surfaces that were used by someone with monkeypox, though this mode isn’t as common
Chang adds that a pregnant person can spread the virus to their fetus through the placenta.
“In the past, most cases of monkeypox were actually in children after contact with infected animals, but that doesn’t seem to be the case with the current outbreak,” Chang adds. “An outbreak in the US in 2003 was traced back to infected prairie dogs.”
Monkeypox is not a sexually transmitted infection. But Erica Susky, an infection control practitioner based in Toronto, says that individuals are incorrectly mislabeling it as such.
“The misconception is that it is a sexually transmitted infection, but close contacts of a non-sexual nature may also be a source of transmission,” says Susky. “For example, close skin-to-skin contact, hugging, kissing, and close face-to-face contact. All of these contacts may not be sexual in nature, though sexual contact is also an opportunity for viral transmission.”
Though monkeypox can be spread sexually, it’s not the primary mode — skin-to-skin contact is — which is why it is not considered an STI.
“This type of monkeypox is rarely fatal,” says Dr. Douglas Chiriboga of Pomona Valley Hospital Medical Center. “The type of monkeypox we are dealing with now is of the West African type.”
But Chiriboga and others caution certain populations are more at risk for fatalities.
“It can be [deadly] for unvaccinated children and immunocompromised populations,” Chang says.
Cox adds that previous outbreaks have seen 1 to 10 percent of the population die.
“Researchers are currently learning more about how to treat the disease and prevent serious complications,” Cox says.
There is currently no known cure for monkeypox, notes Dr. Jay Varma, Kroll’s chief medical advisor, a Kroll Institute Fellow, and the director of the Cornell Center for Pandemic Prevention and Response.
However, there are some treatments. Varma explains that doctors can obtain Tecovirimat (brand-name TPOXX) from the CDC.
“During this outbreak, some patients who have received this drug have reported that it helped clear up their rash faster and reduce their pain substantially,” Varma says.
Cox reiterated that monkeypox is a self-limiting disease.
“Monkeypox generally goes away on its own after two to four weeks,” Cox says. “However, children and those with some medical conditions may become more seriously ill.”
Varma says people are receiving one of two available vaccines for smallpox, which have been shown to be effective against monkeypox:
- ACAM2000, the original smallpox vaccine
- JYNNEOS, a newer vaccine
The vaccine is estimated to be around 85% effective at monkeypox prevention, but the research is currently limited.
“Researchers are doing studies right now on patients during this outbreak to provide a more accurate estimate of how protective the vaccine is in real life,” Varma says.
The CDC
- have been exposed to monkeypox in the past 4 to 14 days
- hold certain occupations, such as laboratory workers who directly handle animals with orthopoxviruses that pose an infection risk to humans
If monkeypox is rarely fatal, why are states declaring emergencies? Why did the
“In most patients, monkeypox causes extreme pain and discomfort for several weeks in many parts of the body,” Varma says. “In some situations, the pain can be so severe that it requires hospitalization, the rash can leave permanent scars on the skin or get infected with bacteria, and/or the disease can cause damage to the brain, eyes, and lungs.”
Varma also notes that for other viruses, including COVID-19, healthcare providers and scientists did not discover other effects until later, such as long COVID-19.
It also poses a more serious risk to vulnerable populations, such as children and immunocompromised, Susky points out.
People with monkeypox are contagious until the rash has completely disappeared, Varma notes.
“This means that a blister has turned into a scab, the scab has formed and fallen off, and new skin is now covering the area where the blister and scab were before,” he says.